A 55 year old female patient came to the OPD with c/o itchy skin lesions over back, hands , neck , face, and fever
CONSENT AND DE-IDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
A 55 year old female patient came to the OPD with
C/o itchy lesions over back,neck,face since 3 months
Initially started over back and progressed to hands
C/o fever since 2 months(one episode per day in the evening)
Complaints of oral ulcers since 1 month
C/o joint pains since 15 days
History of presenting illness
Patient was apparently normal 3 months back And started Having itchy lesions over back its progress to hands,Neck. oral ulcers since one month.High grade fever, one episode per day, relieved on taking medication.Joint pain since 15 days associated with swelling.
No history of morning stiffness.painful oral ulcers since one month, associated with difficulty in swallowing and burning sensation.
History of two episodes of vomiting,Non projectile, non bilious with food particles non blood tinged.
History of three episodes of diarrhea per day for two days, which is water in consistency. No occult blood is present in stools. No history of new drug intake prior to symptom.
No history of dry eyes,Mouth Reynauds phenomenon.
History of swelling of face One month back.
No H/o chestpain,Dyspnea,palpitations
H/o photosensivity present
H/o elephantiasis of right leg since 25yrs
H/o diarrhoea and vomiting since 15 days
Denovo detected hypothyroidism
H/o usage Tab.omnacortil 30mg,T.Augmentin 625mg,Betamethasone lotion
Elephantiasis of right leg before 20 years
GENERAL EXAMINATION
Pt is c/c/c
Afebrile on touch
PR:70 bpm
BP:130/70 mm hg
RR:26 cpm
GRBS:106mg/dl
No Pallor, Icterus, cyanosis, clubbing lymphadenopathy.
SYSTEMIC EXAMINATION
Respiratory system:
Inspection:
No Tracheal deviation.
Chest bilaterally symmetrical
Type of respiration: thoraco abdominal.
No dilated veins,pulsations,scars, sinuses.
No drooping of shoulder.
Palpation:
No Tracheal deviation
Apex beat- 5th intercoastal space,medial to midclavicular line.
Tenderness over chestwall- absent.
Vocal fremitus- Mammary,Infra Axillary and Infrascapular- Decreased on both sides.
Percussion:
Resonant note on all areas
Auscultation:
NVBS,BAE +
Cardiovascular system:
Inspection : no visible pulsation , no visible apex beat , no visible scars.
Palpation: all pulses felt , apex beat felt.
Percussion: heart borders normal.
Auscultation:
Mitral area, tricuspid area, pulmonary area, aortic area- S1,S2 heard.
P/A:Soft ,Non-tender
CNS:
HMF-Intact
Memory -recent and remote:Intact
Speech-Normal
Cranial Nerves -Normal
Motor Examination-
Tone. UL. N. N
LL. N. N
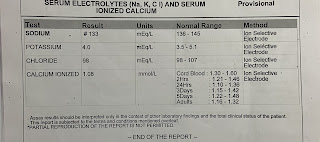
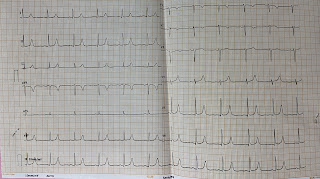
Investigations














Comments
Post a Comment