.Case Scenario - A 55 year old woman from Nalgonda came to OPD on 3rd of June with chief complaints of:-pain abdomen , bilateral upper and lower limb swelling since 10 days and nausea since 1 week.
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
Case Scenario - A 55 year old woman from Nalgonda came to OPD on 3rd of June with chief complaints of:-pain abdomen , bilateral upper and lower limb swelling since 10 days and nausea since 1 week.
History of Presenting Illness-
patient was apparently asymptomatic 10 days ago when she developed edema in bilateral upper and lower limbs and facial puffiness for which she consulted a local physician and was prescribed medication following which the symptoms subsidised but relapsed again 1 week ago.- since 1 week ago she has been experiencing nausea and dysphagia associated with 1 episode of vomiting after consumption of food which was non-projectile, non-bilious, having food contents.-
h/o SOB Grade 4 since 6 months-
h/o rashes on skin 1 month ago which subsidised spontaneously-
h/o burning micturition -
no h/o fever, diarrhoea, constipation, melena, bleeding, hematemesis.
Past History-
k/c/o HTN since 5 years on regular medication- diabetic on examination - n/k/c/o tuberculosis, CAD, epilepsy, asthma, thyroid disorder- h/o abdominal surgery for mass 30 years ago-
no h/o blood transfusions
Personal History-
married-
used to work as a housemaid before -
mixed diet- reduced appetite-
inadequate sleep-
regular bowels-
burning micturition-
no known allergies- alcohol and tobacco addiction 35 years ago- analgesic abuse since 1 year
Family history
- patients mother had breast cancer- patients brother had MI-
no diabetes mellitus-
no hypertension -
no stroke-
no tuberculosis
- no asthma-
no other hereditary diseases
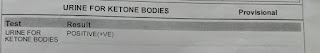
Investigations
USG
patient was conscious, coherent and cooperative-
well built and adequately nourished-
no pallor- no icterus- no cyanosis - no clubbing of fingers- no lymphadenopathy - no pedal edema -
bilateral upper limb edema and facial puffiness present - no malnutrition - no dehydration
Vitals
03/06/23-
BP: 130/90 mm Hg- Pulse rate: 108 bpm-
Respiratory rate24 cpm-
Temperature: afebrile
- SPO2: 98% at RA-
GRBS: 783 mg/dL-04/06/23-
BP: 120/70 mm Hg-
Pulse rate: 88 bpm-
Respiratory rate: 22 cpm-
Temperature: afebrile
- SPO2: 98% at RA-
GRBS: 264 mg/dL
05/06/23-
BP: 110/70 mm Hg-
Pulse rate: 110 bpm-
Respiratory rate: 24 cpm-
Temperature: afebrile -
SPO2: 100% at RA-
GRBS: 181 mg/dL
06/06/23-
BP: 110/80 mm Hg-
Pulse rate: 114 bpm-
Respiratory rate: 22 cpm-
Temperature: afebrile
- SPO2: 96% at RA-
GRBS: 143 mg/dLFluid Intake and Urine Output
Systemic Examination
Cardiovascular System- no thrills-
cardiac sounds S1 and S2 heard-
no cardiac murmurs
Respiratory System- no dyspnea-
no wheeze-
trachea position: central-
breath sounds: vesicular-
no adventitious sounds
Abdomen- shape: obese- no scars, striae, engorgement












Comments
Post a Comment